What is new?
You need to put 100 to 166 employees through an exercise course to prevent a single heart attack in the next 10 years.
Why is this important?
This Number Needed to Treat (NNT) reveals the inefficiency of one-size-fits-all occupational health measures.
What is next?
Individualized lifestyle medicine to replace ‘one size fits all’ courses and interventions. With the objectives to:
- Increase health-related self-competence and self-responsibility outside of the workplace.
- Avoid personnel costs (for course-related loss of working time).
Economic background:
In Germany around 90,000 German citizens of working age between 25 and 64 die annually from lifestyle-related chronic diseases. The consequences for the German economy: a loss of more than 500,000 productive working years every year [1]. That is not all. Chronically ill employees are less productive or altogether absent from the workplace.
That corporate lifestyle interventions can improve the risk of chronic diseases is undisputed [2]. However, all major studies that have not been sponsored by course and service providers fail to show significant improvements in ‘hard indicators’ of monetary value, such as reductions in sick leave and continued pay and increases in productivity in the short term (up to 18 months) [3].
This complicates the determination of a Return on Investment (ROI) for preventive occupational health measures.
One simple indicator illustrates why this is the case: the Number Needed to Treat (NNT). It answers the question of how many participants need to be included in an intervention to avoid, for example, a single cardiovascular event in the next 10 years.
The NNT is calculated as the inverse of absolute risk reduction (ARR), that is:
NNT = 1/ARR
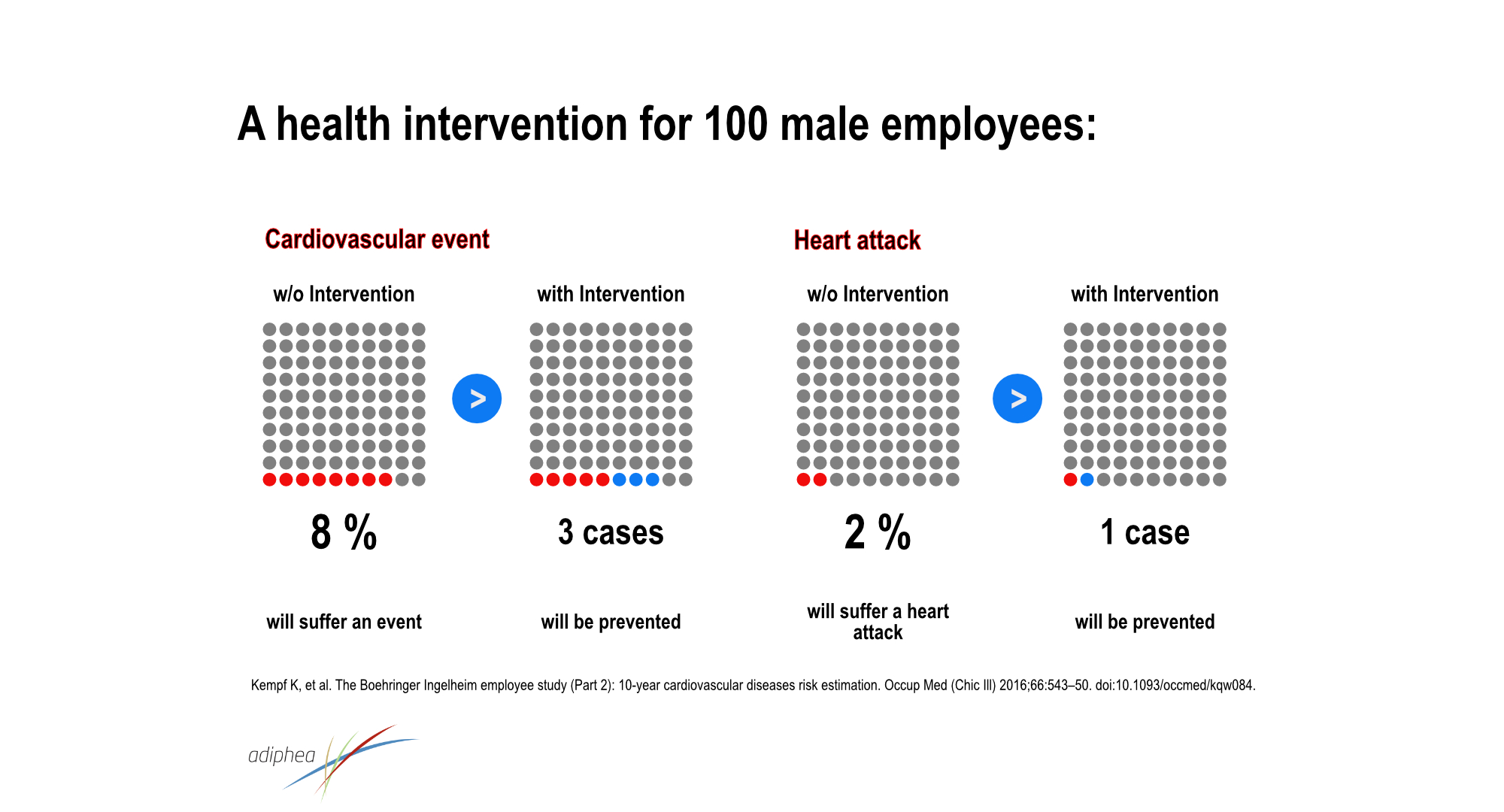
Germany’s largest study on occupational health measures, performed at Boehringer- Ingelheim, one of the largest German pharmaceutical manufacturers, may serve as an illustrative example [4]:
A hypothetical corporate health program that improves blood pressure, HbA1c, HDL cholesterol, triglycerides and C-reactive protein by 10% each, would reduce the absolute risk of a heart attack by 1 percent.
Hence the NNT = 1/0.01 = 100.
That is, 100 (male) employees would need to be enrolled to prevent on heart attack over the next 10 years.
In the BP Europe study, the NNT for a 12-month intervention was even higher: 166 [5]. Unfortunately, scientific articles never present the NNT, but rather the more impressive relative risk reduction [6], which was over 40% in the example of the Boehringer-Ingelheim study.
Beware of return on investment claims from reference studies.
The authors of studies on the effectiveness of occupational health measures regularly present so-called cost-benefit analyses that purport to evaluate the economic efficiency of occupational health promotion. The determined cost-benefit ratios range from 1:2 to 1:19, which corresponds to returns of 100% to 1,800%.
Every corporate decision maker knows that such returns are way above market-standard, and therefore should question the credibility of these calculations.
A research project called ReSuM, funded by the German Federal Ministry of Education and Research, did just that [7].
The authors concluded that the economic analyses applied in tose studies are typically insufficient to prove this miraculous return on investment. Measuring the impact of an occupational health program on employees’ health and valuing it in monetary terms is not only difficult but also subject to errors if, for example, opportunity costs are not considered.
These hyper-optimistic presentations obstruct the view to the real lever for more efficient and effective occupational health promotion: the individualization of preventive measures.
Ironically, this need for individualization becomes apparent in the very studies referenced by occupational health service providers to tout the universal applicability of their courses and interventions [8] [9]. Hidden behind the intervention effect averages are significant inter-individual differences that cover the entire spectrum from very effective to useless or even harmful [10] as illustrated in figure 1.
Figure 1
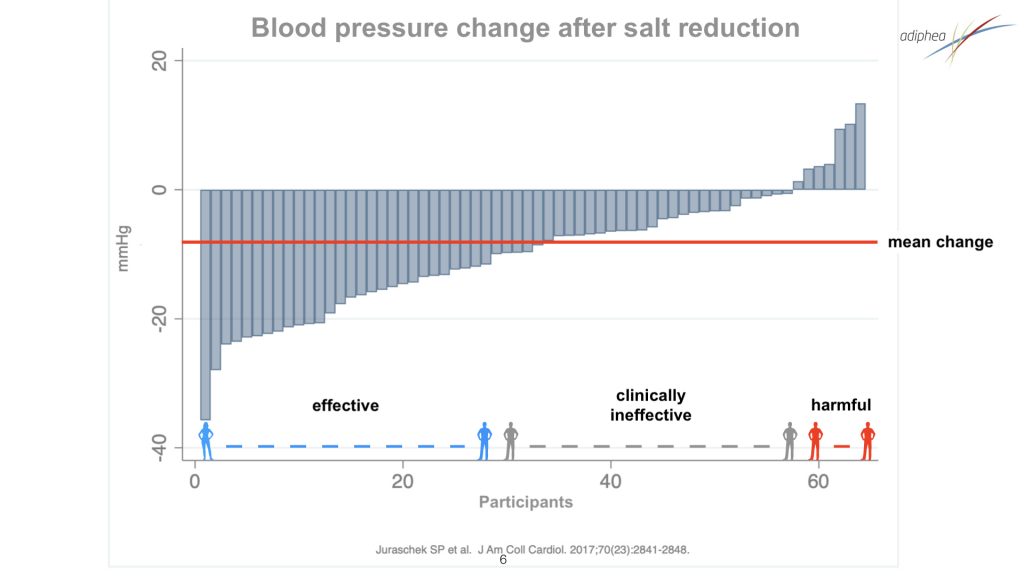
Such studies reliably answer the question of what effect a specific intervention has on a defined target group, but not the question that both the user and the payer of workplace health promotion are interested in: which intervention has the desired effect on a specific employee.
This question can only be answered by a clinically valid N-of-1 study. This is why we make this method accessible to laypeople with LiLo. N-of-1 is the gold standard of experimental single-case research, with the “N” referring to the number of study participants.
Instead of prescribing one-size-fits-all exercise and dietary interventions, LiLo steers the user towards health behaviors that harmonize with their genetic makeup (e.g., exercise, nutrition).
It utilizes the insight that preventable chronic diseases are due to a mismatch between an individual‘s health behavior and their genetic makeup [11].
With respect to the workplace setting, this strategy acknowledges that these behaviors predominantly take place outside the workplace, where each employee spends more than 80% of their time.
With this unorthodox but evidence-based alternative to conventional preventive medicine, significant efficiency gains can be achieved for workplace health promotion:
- Prioritization of health self-competence and -rsponsibility
- Dispensability of on-site courses and coaches
- Avoidance of work time losses (for course-related work time absences)
- Quantitative effectiveness monitoring and control
- Configurability for occupationally relevant disease states (e.g., stress & depression, metabolic syndrome, overweight, hypertension, (pre-)diabetes)
References
[1] OECD/EU 2016. Health at a Glance: Europe 2016 – State of Health in the EU Cycle. OECD Publishing; 2016. doi:10.1787/9789264265592-en.
[2] Nieste I, Franssen WMA, Spaas J, Bruckers L, Hans HC, Savelberg M, et al. Lifestyle interventions to reduce sedentary behaviour in clinical populations : A systematic review and meta-analysis of different strategies and effects on cardiometabolic health. Prev Med (Baltim) 2021;148:106593. doi:10.1016/j.ypmed.2021.106593.
[3] Song Z, Baicker K. Effect of a Workplace Wellness Program on Employee Health and Economic Outcomes: A Randomized Clinical Trial. JAMA – J Am Med Assoc 2019;321:1491–501. doi:10.1001/jama.2019.3307.
[4] Kempf K, Martin S, Döhring C, Dugi K, Haastert B, Schneider M. The Boehringer Ingelheim employee study (Part 2): 10-year cardiovascular diseases risk estimation. Occup Med (Chic Ill) 2016;66:543–50. doi:10.1093/occmed/kqw084.
[5] Schaller N, Blume K, Hornig M, Senker L, Wolfarth B, Schuster T, et al. Occupational life-style programme over 12 months and changes of metabolic risk profile, vascular function, and physical fitness in blue-collar workers. J Occup Med Toxicol 2023;18:1–8. doi:10.1186/s12995-023-00370-w.
[6] Elliott MH, Skydel JJ, Dhruva SS, Ross JS, Wallach JD. Characteristics and Reporting of Number Needed to Treat, Number Needed to Harm, and Absolute Risk Reduction in Controlled Clinical Trials, 2001-2019. JAMA Intern Med 2021;181:282–4. doi:10.1001/jamainternmed.2020.4799.
[7] Gloede D. Betriebliche Gesundheitsförderung und wirtschaftliche Effizienz – Entwicklungsstand und Perspektiven der Wirtschaftlichkeitsevaluation in der Präventionsforschung – 2010;1198.
[8] Rodgers GP, Collins FS. Precision Nutrition—the Answer to “What to Eat to Stay Healthy.” JAMA 2020;324:735–6. doi:10.1001/jama.2020.13601.
[9] Dawson EA, Sheikhsaraf B, Boidin M, Erskine RM, Thijssen DH. Intra-individual differences in the effect of endurance vs. Resistance training on vascular function: a cross-over study. Scand J Med Sci Sports 2021. doi:10.1111/sms.13975.
[10] Juraschek SP, Miller ER, Weaver CM, Appel LJ. Effects of Sodium Reduction and the DASH Diet in Relation to Baseline Blood Pressure. J Am Coll Cardiol 2017;70:2841–8. doi:10.1016/j.jacc.2017.10.011.
[11] Kraushaar LE, Bauer P. Dismantling Anti-Ageing Medicine: Why Age-Relatedness of Cardiovascular Disease is Proof of Robustness Rather Than of Ageing-Associated Vulnerability. Hear Lung Circ 2021;30:1702–9. doi:10.1016/j.hlc.2021.05.105.