What’s new
The health recommendations that are portrayed as universally valid are typically very effective for some, not really effective for many, and even harmful for a few.
Why is this important?
Because a healthcare system worthy of the name should make individualized lifestyle medicine available to everyone.
The solution
Individualised lifestyle medicine operationalised for lay-users, with real-time feedback.
One-size-does-not-fit-all
While cookies spike blood sugar for some people and bananas don’t, it’s the opposite for others [1].
Two people eat the same bread but have a blood sugar response that is 8-fold different [1].
Less salt in food reduces blood pressure in some, leaves it unchanged in many, and drives it up in quite a few [2].
And the same amount of exercise makes some fitter than others [3].
These clinical findings illustrate that health recommendations shouldn’t pretend to be one-size-fits-all.
The reason for these differences are the inextricably complex interactions between behavior, heredity, metabolism, microbiome, and environment.
N-of-1 as the alternative to one-size-fits-all
Without real-time feedback about the effects of health behaviors on the biomarkers that determine lifelong vitality and function, no one can know which health habits will ensure chronic health and function throughout life.
The solution is turn oneself into a clinical trial. The tool to do this is called self-experimentation.
What sounds adventurous, even rebellious, to health bureaucrats is in fact completely legitimate.
For two reasons:
First, a health care system that accepts its own health recommendations to be ineffective for many, and even harmful for some, must also accept these health recommendations to be taken for a “test drive”.
Second, the method of “test driving”, the so-called N-of-1 study is legitimized as the gold standard of single-case research by EMA (European Medicines Agency) and FDA (Food and Drug Administration) [4,5].
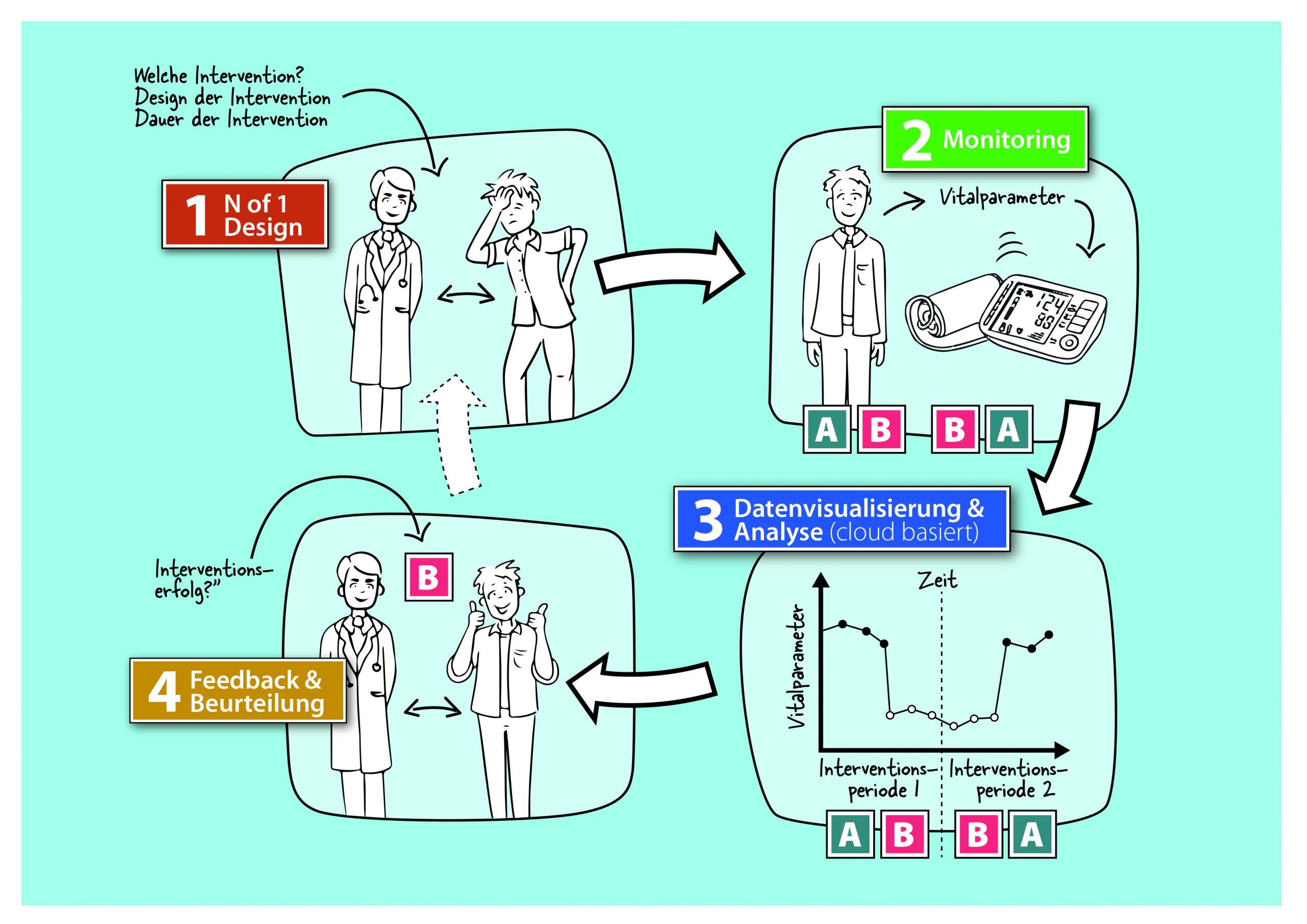
With the N-of-1 study design, a single subject becomes their own clinical trial (the “N” in trials stands for the number of participants) in which he or she simultaneously acts as his or her own control and intervention “group.”
What determines the quality and significance of an N-of-1 study is the repeated (usually daily) measurement of a relevant biomarker (e.g. blood pressure) in successive control and treatment phases (AB phases; A = placebo, B = verum), each lasting several days or a few weeks.
Special statistical methods can then be applied to infer from the measurement data whether the intervention is effective and how large its effect is.
N-of-1 comes in different configurations. The simplest being the AB design that has a single phase change. Better than having only one phase change are two phase changes (ABA) or three (ABAB). This fits well with interventions that can alternately be applied and suspended, such as eating less salt.
But for those, for example, who have finally gotten around to adopting some regular exercise routine (in the B-phase), there shouldn’t be another A-phase of suspending this routine, otherwise it will not become a habit.
For such constellations, ABCD configurations are suitable, in which only the volume or intensity of the intervention is changed.
These are only two examples from the N-of-1 compendium, for which special statistical methods have been developed.
The N-of-1 toolbox for everyone
In our health care system, N-of-1 is (still) ignored [6,7]. This is because physicians’ offices neither have the time for daily measurement nor the methodological expertise to analyze the collected data.
This is a pity, because with mobile health technologies (e.g., WLAN-enabled blood pressure monitors) and server-based IT platforms, the N-of-1 method can be operationalized so that any layperson can use it.
And that is precisely why we created LiLo. So that everyone can have access to individualised lifestyle medicine today – with feedback in real time.
Because if you want to ensure lifelong health and functionality, you need to know today where you’re headed.
With the systematic trial-and-error method of N-of-1, it is not only possible to precisely match one’s lifestyle to one’s genetic makeup.
You also discover whether you really need to cut back on cookies and bread, and how much exercise is enough for lifelong health and functionality.
So why blind flying your efforts to lifelong health and function when individualised lifestyle medicine is available in N-of-1 precision?
References
[1] Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, et al. Personalized Nutrition by Prediction of Glycemic Responses. Cell 2015;163:1079–94. doi:10.1016/j.cell.2015.11.001.
[2] Felder RA, Gildea JJ, Xu P, Yue W, Armando I, Carey RM, et al. Inverse Salt Sensitivity of Blood Pressure: Mechanisms and Potential Relevance for Prevention of Cardiovascular Disease. Curr Hypertens Rep 2022;24:361–74. doi:10.1007/s11906-022-01201-9.
[3] Pickering C, Kiely J. Do Non-Responders to Exercise Exist—and If So, What Should We Do About Them? Sport Med 2019;49:1–7. doi:10.1007/s40279-018-01041-1.
[4] European Medicines Association. Guideline on Clinical Trials in Small Populations. 2006.
[5] Nikles J, Onghena P, Vlaeyen JWS, Wicksell RK, Simons LE, Mcgree JM, et al. Establishment of an International Collaborative Network for N-of-1 Trials and Single-Case Designs. Contemp Clin Trials Commun 2021;23:100826. doi:10.1016/j.conctc.2021.100826.
[6] Wicks P. Patient, study thyself. BMC Med 2018;16:217. doi:10.1186/s12916-018-1216-2.
[7] Schork NJ. Personalized medicine: Time for one-person trials. Nature 2015;520:609–11. doi:10.1038/520609a.